Essential oils are aromatic, volatile liquids extracted from plant material by steam distillation and named for the plants from which they are derived.1 Essential oils are readily available in pharmacies, supermarkets, health food stores, and online. In 2017, 11% of Australians reported using essential oils for medicinal purposes in the previous year;2 the major reported sources of advice were general practitioners (10%) or pharmacists (18%), while 43% of oils were self‐prescribed.2
Essential oils are typically used topically or added to vaporisers, but oral ingestion of small amounts is recommended by some suppliers. They can, however, cause severe toxicity when ingested, the risk depending on the oil used; the onset of toxicity can be rapid, and small quantities (as little as 5 mL) can cause life‐threatening toxicity in children.3 Clinical effects include vomiting, central nervous system depression or excitation, and aspiration pneumonitis.3 Increasing frequency4 and severity5 of essential oil poisonings have been reported in Europe and the United States.
We conducted a retrospective study of essential oil exposure calls to the New South Wales Poisons Information Centre (NSWPIC) during July 2014 – June 2018. NSWPIC takes about half of all calls to Poisons Information Centres in Australia. We characterised essential oil exposures, including the essential oils involved and changes over time, the demographic characteristics of exposed persons, and seasonality. Change over time was assessed by Poisson regression in SAS 9.3. The Human Research Ethics Committee of the Sydney Children's Hospitals Network approved the study (reference, LNR/16/SCHN/44).
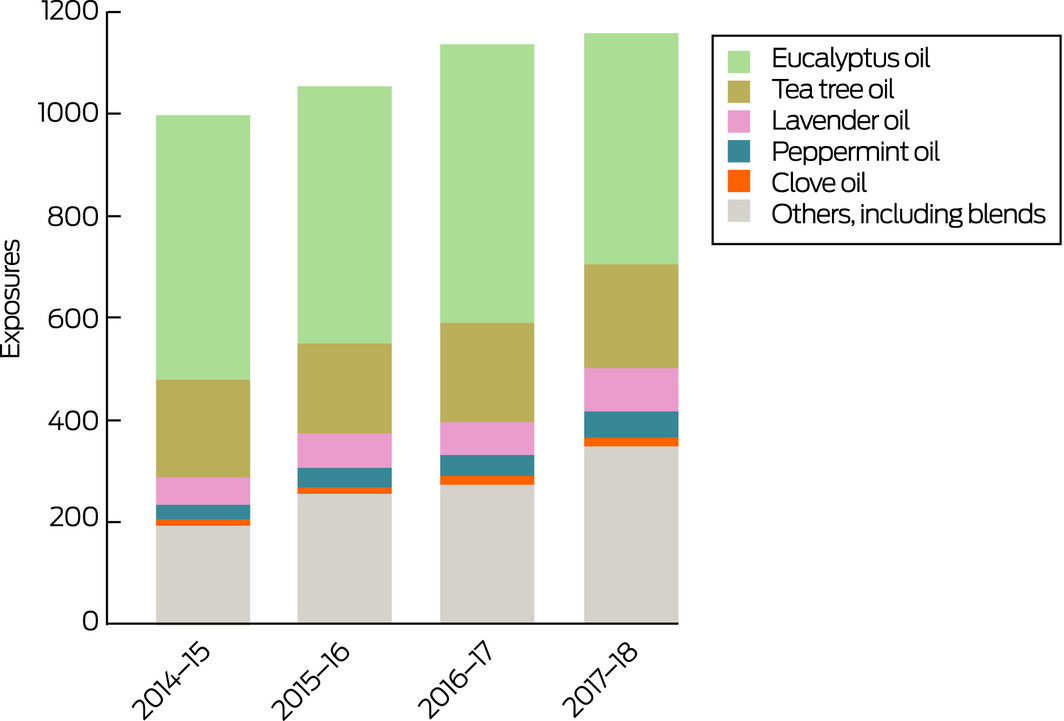
We identified 4412 essential oil exposures reported to NSWPIC during the 4‐year study period; 1387 callers (31%) had symptoms of poisoning at the time of the call. The number of calls increased from 1011 in 2014–15 to 1177 in 2017–2018 (16.4% increase, or 5.3% per year; 95% confidence interval, 2.6–8.1% per year) (Box 1). Most exposures were accidental (3530, 80%) or the results of therapeutic error (580, 13%), typically mistaking essential oils for liquid pharmaceuticals, usually cough liquids (84, 14%); there were 105 cases (2.4%) of misinformed misuse (eg, intended ingestion of essential oils with therapeutic intent). In 2790 cases (63%), the exposed person was under 15 years of age (Box 2).
The essential oils most frequently involved in poisonings were eucalyptus (2049, 46.4%), tea tree (749, 17.0%), lavender (271, 6.1%), clove (179, 4.1%), and peppermint oils (154, 3.5%). Reported eucalyptus oil exposures were more frequent during winter months (June–August: 54.3 calls per month; 38.7 calls per month in other seasons).
We found that essential oil exposures are frequent in Australia, and that more than half involve children. We identified a small subset of cases of misinformed misuse (intentional ingestion for perceived health benefits). Exposures are increasing in number, perhaps reflecting increased use of essential oils and indicating the need for public education. Safe storage is important, and we recommend that essential oils be kept separate from oral medications to prevent therapeutic errors. Flow restrictors and child‐resistant closures would be desirable, but containers are only required to have such closures when the essential oil volume exceeds 15 mL; as severe toxicity can be caused by as little as 5 mL, this is inadequate for protecting children. Health care professionals and members of the public can receive advice about essential oil exposures from the Poisons Information Centre on 131126 (24 hours, Australia‐wide).
Box 1 – Essential oil exposures reported to the New South Wales Poisons Information Centre, 2014–2018
Box 2 – Demographic characteristics of exposed persons in 4412 essential oil exposure calls to the New South Wales Poisons Information Centre, 2014–2018
|
Characteristic |
|
||||||||||||||
|
|
|||||||||||||||
|
Age |
|
||||||||||||||
|
Neonate (0–4 weeks) |
13 (0.3%) |
||||||||||||||
|
Infant (4 weeks to 1 year) |
312 (7.1%) |
||||||||||||||
|
Toddler (1–4 years) |
2179 (49.4%) |
||||||||||||||
|
Child (5–14 years) |
286 (6.5%) |
||||||||||||||
|
Adolescent (15–19 years) |
58 (1.3%) |
||||||||||||||
|
Adult (20–74 years) |
1428 (32.4%) |
||||||||||||||
|
Older adult (75 years or more) |
130 (2.9%) |
||||||||||||||
|
Unknown |
6 (0.1%) |
||||||||||||||
|
Sex |
|
||||||||||||||
|
Female |
2340 (53.0%) |
||||||||||||||
|
Male |
2021 (45.8%) |
||||||||||||||
|
Unknown |
51 (1.2%) |
||||||||||||||
|
Exposure type |
|
||||||||||||||
|
Accidental |
3530 (80.0%) |
||||||||||||||
|
Therapeutic error |
580 (13.1%) |
||||||||||||||
|
Intentional |
192 (4.4%) |
||||||||||||||
|
Adverse reaction |
79 (1.8%) |
||||||||||||||
|
Other |
31 (0.7%) |
||||||||||||||
|
Disposition |
|
||||||||||||||
|
Referred to hospital |
365 (8.3%) |
||||||||||||||
|
Call originated from hospital |
363 (8.2%) |
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 12 June 2019, accepted 8 August 2019
- 1. Ríos JL. Essential oils: what they are and how the terms are used and defined. In: Preedy VR, editor. Essential oils in food preservation, flavor and safety. Amsterdam: Elsevier, 2015; pp. 3–10.
- 2. Harnett JE, McIntyre E, Steel A, et al. Use of complementary medicine products: a nationally representative cross‐sectional survey of 2019 Australian adults. BMJ Open 2019; 9: e024198.
- 3. Woolf A. Essential oil poisoning. J Toxicol Clin Toxicol 1999; 37: 721–727.
- 4. Janes SEJ, Price CSG, Thomas D. Essential oil poisoning: N‐acetylcysteine for eugenol‐induced hepatic failure and analysis of a national database. Eur J Pediatr 2005; 164: 520–522.
- 5. Mowry JB, Spyker DA, Brooks DE, et al. 2015 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd annual report. Clin Toxicol 2016; 54: 924–1109.





We thank staff at the New South Wales Poisons Information Centre for their contributions to the NSWPIC database.
No relevant disclosures.