Injury prevention is one of the Australian National Health Priority Areas.1 Injuries requiring medical attention place considerable demands on the health care system and are increasingly being recognised as a significant public health problem.2 Recent statewide data from Victoria show that the public health burden of sports injury, as a particular context for hospitalised injury, has increased significantly in recent times.3,4 Understanding whether sports injury rates vary by geographic regions in Vic would inform better health service delivery to redress identified health inequalities across regions and aid targeting of preventive programs.
Analysis of International Classification of Diseases-coded hospitalisation data routinely collected from all Victorian public and private hospitals admissions over the financial years 2003–04 to 2011–12 was undertaken. The cases selected had a principal diagnosis of injury and an activity code indicating sport. They were classified according to the Local Government Area (LGA; 31 metropolitan, 49 rural/regional) of the patients’ usual residence. Population-adjusted sports injury hospital admission rates were based on annual LGA populations; trends were analysed by negative binomial regression.
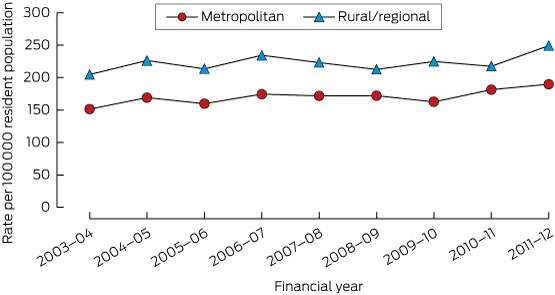
The overall annual number of sports injury-related hospital admissions increased by 34% (n = 8092 to n = 11 359). The regression model found a corresponding 15% increase in the annual population-adjusted sports injury-related hospital admissions rate from 166.0 to 205.01 per 100 000 population. For every year, the population-adjusted rate of sports injury hospital admissions was higher for people residing in rural/regional LGAs than in metropolitan LGAs (Box, Appendix).
Sports injuries requiring hospital treatment can have a significant impact on individuals and for the health services providing the treatment, particularly in rural/regional communities. Our data demonstrate geographical differences in population-adjusted sports injury hospital admissions rates that have persisted over time. This epidemiological study is the first step to understanding how the burden of sports injuries varies by region in Victoria.
Our findings are likely to be an underestimation of the geographical variations in sports injury health care burden. Only a small proportion of people who sustain a sports injury are admitted to hospital; however, research has shown that a substantial number of sports injuries receive some form of health care treatment.5 The higher rate of sports injury hospital admissions for people residing in rural/regional areas could be due to a number of factors that are different for people residing in metropolitan areas: hospital administrative practices, health care accessibility, level/nature of sports injury risk, or sports participation levels.
In conclusion, these findings have implications for strategic planning around availability of trained staff in rural/regional health services to meet the demands for sports injuries requiring hospital treatment. There is a need for further research that links location of the injury occurrence to the LGA of treating health service and the LGA of residence to explain these geographical variations in sports injury burden more accurately.
Received 20 May 2015, accepted 11 August 2015
- 1. Commonwealth Department of Health and Family Services and Australian Institute of Health and Welfare. National Health Priority Areas Report: Injury Prevention and Control 1997. Canberra: Australian Institute of Health and Welfare, 1998. (AIHW Cat. No. PHE 3.) http://www.aihw.gov.au/publication-detail/?id=6442466968 (accessed Jun 2015).
- 2. Pointer S. Trends in hospitalised injury, Australia: 1999-00 to 2010-11. Canberra: Australian Institute of Health and Welfare, 2013. (AIHW Cat. No. INJCAT 162.) http://www.aihw.gov.au/publication-detail/?id=60129544399 (accessed Jun 2015).
- 3. Finch CF, Wong Shee A, Clapperton A. Time to add a new priority target for child injury prevention? The case for an excess burden associated with sports and exercise injury: population-based study. BMJ Open 2014; 4: e005043.
- 4. Finch CF, Kemp JL, Clapperton AJ. The incidence and burden of hospital-treated sports-related injury in people aged 15+ years in Victoria, Australia, 2004-2010: a future epidemic of osteoarthritis? Osteoarthritis Cartilage 2015; 23: 1138-1143.
- 5. Mitchell R, Finch C, Boufous S. Counting organised sport injury cases: evidence of incomplete capture from routine hospital collections. J Sci Med Sport 2010; 13: 304-308.





Anna Wong Shee was supported by a Robert HT Smith Postdoctoral Fellowship at Federation University Australia. Angela Clapperton was supported by the Victorian Injury Surveillance Unit core grant from the Victorian Department of Health and by research funding from the International Olympic Committee as part of infrastructure support for the Australian Centre for Research into Injury in Sport (ACRISP). Caroline Finch was supported by a National Health and Medical Research Council Principal Research Fellowship (ID: 1058737). ACRISP is one of the International Research Centres for Prevention of Injury and Protection of Athlete Health supported by the IOC.
No relevant disclosures.