We report the first recognised case of infection with Clostridium difficile PCR ribotype 027 acquired in Australia. This pathogen has caused significant morbidity and mortality in widespread hospital-based outbreaks in the northern hemisphere. Clinicians need to be aware of the clinical picture, limitations of diagnostic tests, availability of further testing for epidemic strains, new therapeutic approaches, and in-hospital control strategies for this infection. (MJA 2011; 194: 369-371)
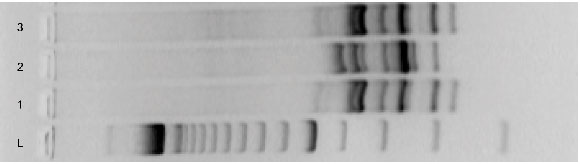
Repeat stool specimens were tested. This time, C. difficile toxins were identified by enzyme-linked fluorescent assay, and C. difficile was isolated again. Because of the patient’s deteriorating condition, the laboratory was alerted to the possibility of a hypervirulent strain. The isolate was tested for susceptibility to moxifloxacin (Etest, bioMérieux, Sydney, NSW) and found to be resistant, with a minimum inhibitory concentration of > 32 μg/L. The stool sample was positive by real-time polymerase chain reaction (PCR; GeneXpert, Cepheid, Sunnyvale, Calif, USA) when tested for the presence of C. difficile organisms carrying genes for toxin B (tcdB), binary toxin (cdtB) and an 18-base-pair deletion within the tcdC gene that is characteristic of the PCR ribotype 027 strain. These findings were confirmed by sequencing the tcdC gene, and this also identified a point mutation at nucleotide position 117, which is also characteristic of this strain. PCR ribotyping was undertaken using a previously published method1 that confirmed the isolate as PCR ribotype 027 (Box).
An epidemic strain of C. difficile (PCR ribotype 027) was first identified in Quebec Province in Canada in 2005, as a cause of hospital outbreaks of severe infection with high mortality rates.2 Retrospective analyses suggested that this strain had caused outbreaks across North America since 2000.3 The organism later spread to Europe, and cases have now been described in Asia and Central America.4 Increased toxin production by C. difficile PCR ribotype 027 may be responsible for its increased virulence,5 and fluoroquinolone resistance is likely to be contributing to its spread.6 Infection with this strain more often leads to severe disease, and is associated with more recurrences and a greater risk of death.2 Until now, only one case has been described in Australia in a patient who was thought to have acquired the infection in North America.7
This is the first case of hypervirulent CDI diagnosed in Australia with apparent local acquisition. Several factors support the conclusion that the infection was not acquired overseas. First, although the patient had travelled to Latvia 4 months before being admitted, the possibility that he acquired C. difficile PCR ribotype 027 then and remained colonised is remote. C. difficile does not colonise the normal adult gastrointestinal tract, and the patient received no antibiotics that may have disrupted his gut flora in the time between returning from Latvia and admission to hospital. Second, a recent publication from Latvia indicates that C. difficile ribotype 027 was not present in the country when our patient was there.8 Finally, there were at least two other subsequently confirmed cases of infection with C. difficile PCR ribotype 027 in the hospital at the time the patient developed symptoms of infection (it is not known where these cases were acquired).
The case illustrates important features of hypervirulent CDI. The identification of severe disease is critical in guiding management. For surveillance purposes, severe disease may be simply identified as infections requiring ICU admission or surgery, or infections resulting in death, or a diagnosis of toxic megacolon.9 More sensitive diagnostic criteria for severe disease in addition to those above are required to guide patient care. While no such criteria have yet been prospectively validated, proposed markers of severe disease include age greater than 65 years, leukocytosis greater than 20 × 109 cells/L, deterioration of renal function, temperature greater than 38.3°C, serum albumin concentration less than 25 g/L and an elevated serum lactate concentration.10 Our patient met all these criteria except for the serum lactate concentration, which was not recorded.
Although metronidazole remains the recommended first-line agent for mild to moderate CDI, oral vancomycin is now recommended for severe disease.9,10 Although there is no evidence that high-dose oral vancomycin (500 mg, 6-hourly) is any better than standard doses of 125 mg 6-hourly, higher doses are favoured by many clinicians. Evidence of benefit for vancomycin enemas is limited to case series; eight of nine patients with refractory severe disease had complete resolution with this therapy.11 In the setting of ileus with toxic megacolon, oral vancomycin will not reach the colon and intravenous delivery of metronidazole is preferable.12
Surgery should be considered if severe disease is unresponsive to medical therapy after 48 hours, or if there is bowel perforation or multiorgan failure.13 Elevation of plasma lactate to between 2.2 and 4.9 mmol/L has been identified in a retrospective review of a selected group of severely ill patients as a guide to when colectomy is most beneficial.14 Other strategies requiring further investigation for use in severe disease include intravenous immunoglobulin, alternative antibiotics such as tigecycline, and monoclonal antibodies.
C. difficile spores are highly resistant to killing by alcohol and most other disinfectants. In outbreaks of CDI, health care workers should be instructed to wash their hands with soap and water in addition to using alcohol-based hand disinfection when caring for infected patients. Patients should be isolated and contact precautions with gowns and gloves are recommended. Environmental cleaning with hypochlorite-based solutions is necessary to eliminate the spores.9 Antibiotic stewardship is also an important element in control strategies, with studies of antibiotic restriction showing benefit.15
In Australia, laboratory diagnosis of CDI is most commonly made through detection of C. difficile toxins A and B using enzyme immunoassay (EIA) kits. EIA kits have reported sensitivities of 75%–95%, but most of the evaluations reporting these sensitivities use faecal cytotoxin detection (a flawed test) as the gold standard.16 In addition, the positive predictive value of these tests declines markedly in situations where the prevalence of disease is low.16 Poor sensitivity of the assay is the likely explanation for the initial negative result of the enzyme-linked fluorescent assay in our case. Despite this limitation, EIA kits remain widely used because of their simplicity and relatively low cost. Commercial real-time PCR testing for toxin genes (usually tcdB), has better sensitivity (93%) and specificity (97%),16 and is now available in several Australian laboratories. Toxigenic culture — isolation of the organism followed by toxin testing of the isolate — is extremely sensitive, but it is labour intensive and takes at least 3 days.16 There is currently great debate about the value of an algorithmic approach to diagnosing CDI, whereby a sensitive screening test is used to screen out negatives, thus improving the positive predictive value of a secondary test, particularly when the prevalence of infection is low.17
Distinguishing C. difficile PCR ribotype 027 from other strains of C. difficile does not affect individual patient management, but is important for surveillance purposes. Some commercially available PCR methods can presumptively identify PCR ribotype 027 based on detection of binary toxin genes and the characteristic 18-base-pair deletion in the tcdC gene. An alternative, less expensive, approach is to screen for moxifloxacin resistance by using a 5 μg moxifloxacin disc on a lawn culture of C. difficile on Mueller-Hinton agar. Worldwide, most PCR ribotype 027 isolates are resistant to moxifloxacin,2 while, in Australia, the prevalence of resistance in all strains of C. difficile is 1%. (T V Riley, B Elliot and colleagues, unpublished data). Zones of inhibition for resistant strains (potentially PCR ribotype 027) are > 16 mm while for susceptible strains, they are ≥ 16 mm (T V Riley and colleagues, unpublished data). Isolates of moxifloxacin-resistant C. difficile identified in this way can then be sent for further typing.
With the identification of the first case of PCR ribotype 027 C. difficile infection acquired locally, it is important that clinicians in Australia are aware of the clinical picture, limitations of diagnostic tests, availability of further testing for PCR ribotype 027, new therapeutic approaches,18 and in-hospital control strategies for this infection.19 The solution to the bigger problem of the emergence of virulent strains of C. difficile continues to lie in the basics of surveillance, antimicrobial stewardship, infection control and environmental cleanliness.
Provenance: Not commissioned; externally peer reviewed.
- 1. O’Neill GL, Ogunsola FT, Brazier JS, Duerden BI. Modification of a PCR-ribotyping method for application as a routine typing scheme for Clostridium difficile. Anaerobe 1996; 2: 205-209.
- 2. Loo VG, Poirier L, Miller MA, et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N Engl J Med 2005; 353: 2442-2449.
- 3. McDonald LC, Killgore GE, Thompson A, et al. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med 2005; 353: 2433-2441.
- 4. Clements CAA, Soares Magalhães RJ, Tatem AJ, et al. Clostridium difficile polymerase chain reaction ribotype 027: assessing the risks of further global spread. Lancet Infect Dis 2010; 10: 395-404.
- 5. Warny M, Pepin J, Fang A, et al. Toxin production by an emerging strain of Clostridium difficile associated with outbreaks of severe disease in North America and Europe. Lancet 2005; 366: 1079-1084.
- 6. Pepin J, Saheb N, Coulombe M-A, et al. Emergence of fluoroquinolones as the predominant risk factor for Clostridium difficile-associated diarrhea: a cohort study during an epidemic in Quebec. Clin Infect Dis 2005; 41: 1254-1260.
- 7. Riley TV, Thean S, Hool G, Golledge CL. First Australian isolation of epidemic Clostridium difficile PCR ribotype 027. Med J Aust 2009; 190: 706-708. <MJA full text>
- 8. Aksenoka K, Balode A, Grope I, et al. Clostridium difficile associated disease clinical and molecular data. Acta Chirurgica Latviensis 2009; 9: 56-61.
- 9. Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol 2010; 31: 431-455.
- 10. Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis 2007; 45: 302-307.
- 11. Apisarnthanarak A, Razavi B, Mundy LM. Adjunctive intracolonic vancomycin for severe Clostridium difficile colitis: case series and review of the literature. Clin Infect Dis 2002; 35: 690-696.
- 12. Bolton RP, Culshaw MA. Faecal metronidazole concentrations during oral and intravenous therapy for antibiotic associated colitis due to Clostridium difficile. Gut 1986; 27: 1169-1172.
- 13. Miller MA. Clinical management of Clostridium difficile-associated disease. Clin Infect Dis 2007; 45 Suppl 2: S122-S128.
- 14. Lamontagne F, Labbe AC, Haeck O, et al. Impact of emergency colectomy on survival of patients with fulminant Clostridium difficile colitis during an epidemic caused by a hypervirulent strain. Ann Surg 2007; 245: 267-272.
- 15. Thomas C, Stevenson M, Williamson DJ, Riley TV. Clostridium difficile-associated diarrhoea: epidemiological data from Western Australia following a change in antibiotic policy. Clin Infect Dis 2002; 35: 1457-1462.
- 16. Planche T, Aghaizu A, Holliman R, et al. Diagnosis of Clostridium difficile infection by toxin detection kits: a systematic review. Lancet Infect Dis 2008; 8: 777-784.
- 17. Wilcox MH, Planche T, Fang FC. What is the current role of algorithmic approaches for diagnosis of Clostridium difficile infection? J Clin Microbiol 2010; 48: 4347-4353.
- 18. Cheng AC, Ferguson JK, Richards MJ, et al. Australasian Society for Infectious Diseases guidelines for the diagnosis and treatment of Clostridium difficile infection. Med J Aust 2011; 194: 000-000. <MJA full text>
- 19. Stuart RL, Marshall C, McLaws ML, et al. ASID/AICA position statement: infection control guidelines for patients with Clostridium difficile infection in health care settings. Healthcare Infect 2011. In press.





Thanks to Grant Jenkin of the Department of Infectious Diseases, Monash Medical Centre for his assistance with collation of laboratory data.
Thomas Riley has undertaken contract research for Cepheid.