Clinical record
Inclusion body myositis. This late-onset inflammatory muscle disease results in impaired muscle function, muscle atrophy and weakness, affecting both proximal and distal muscles. It accounts for 17%–30% of idiopathic inflammatory myopathies and can be associated with autoimmune diseases.2-4 In the past, patients with myositis were discouraged from exercising owing to a fear of increased muscle inflammation. However, studies in the 1990s reported that exercise might have a non-specific benefit.5 Patients with inflammatory muscle disease benefit from mild to moderate muscle training and endurance exercise, and muscle inflammation does not increase after exercise.6-8 A specifically tailored rehabilitation program improved our patient’s physical function without evidence of increased muscle damage.
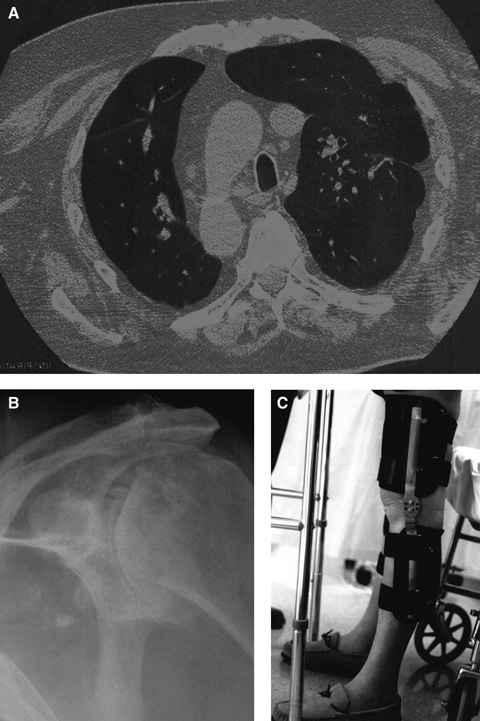
Interstitial pulmonary fibrosis. This group of lung diseases affects the interstitium of the lungs, eventually causing restrictive lung disease. Pulmonary rehabilitation — involving strength and endurance training for arm and leg muscles (eg, walking, cycling, lifting small weights), education on energy conservation and anxiety management, chest physiotherapy, and breathing techniques such as pursed lip and diaphragmatic breathing — has been shown to reduce dyspnoea, improve exercise capacity, enhance quality of life and reduce hospitalisation.9
Chronic shoulder pain from arthritis. This type of pain can be safely and effectively treated by suprascapular nerve block, which avoids the side effects of oral analgesics.10 In our patient, it was an essential component of the rehabilitation program because it enabled him to perform activities of daily living and use a walking frame. Intra-articular steroid injection was not used as it might have worsened the avascular necrosis of the head of the left humerus.
Genu recurvatum. This is an angular deformity (hyperextension at the knee) in the sagittal plane caused by quadriceps weakness. Mediolateral (valgus and varus) instability occurs in the coronal plane. Both deformities require three-point stabilisation. In our patient, orthoses with a free-motion joint and a hyperextension block controlled both deformities and allowed knee movement during walking.11 Gait training with such orthoses includes static weight shift and dynamic balancing exercise in parallel bars, followed by progression to a normal gait pattern.
Lessons from practice
Patients with inflammatory muscle disease benefit from mild to moderate muscle training and endurance exercise.
The goals of multidisciplinary rehabilitation are to restore function and to enhance quality of life.
Active rehabilitation should always be considered, regardless of the apparent severity of underlying medical conditions.
- 1. MacDermid JC, Solomon P, Prkachin K. The Shoulder Pain and Disability Index demonstrates factor, construct and longitudinal validity. BMC Musculoskelet Disord 2006; 7: 12.
- 2. Carpenter S, Karpati G, Heller I, Eisen A. Inclusion body myositis: a distinct variety of idiopathic myopathy. Neurology 1978; 28: 8-17.
- 3. Lotz BP, Engel AG, Nishimo H, et al. Inclusion body myositis. Observations in 40 patients. Brain 1989; 112: 727-747.
- 4. Rugiero M, Koffman B, Dalakas MC. Association of inclusion body myositis with autoimmune and autoantibodies. Ann Neurol 1995; 38: 333.
- 5. Von der Kooi EL, Lindeman E, Riphagen I. Strength training and aerobic exercise training for muscle disease. Cochrane Database Syst Rev 2005; (1): CD003907.
- 6. Alexanderson H, Lundberg IE. The role of exercise in the rehabilitation of idiopathic inflammatory myopathies. Curr Opin Rheumatol 2005; 17: 164-171.
- 7. Varju C, Petho E, Kutas R, Czirjak L. The effect of physical exercise following acute disease exacerbation in patients with dermato/polymyositis. Clin Rehabil 2003; 17: 83-87.
- 8. Arnardottir S, Alexanderson H, Lundberg H, Borg K. Sporadic inclusion body myositis: pilot study on the effects of a home exercise program on muscle function, histopathology and inflammatory reaction. J Rehabil Med 2003; 35: 31-35.
- 9. Abramson MJ, Crockett PA, McDonald CF. COPDX: an update of guidelines for the management of chronic obstructive pulmonary disease with a review of recent evidence. Med J Aust 2006; 184: 342-345.
- 10. Shanahan EM, Ahern M, Smith M, et al. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Ann Rheum Dis 2003; 62: 400-406.
- 11. Datta Gupta A, Mahalanabis D. Genu recurvatum in hemophilia: a case report. Arch Phys Med Rehabil 2007; 88: 791-793.





We acknowledge Maree Braithwaite (Occupational Therapist), Nicolle Datson (Physiotherapist) and Jessica Quayle (Orthotist) of St Margaret’s Rehabilitation Hospital for assisting in the management of our patient. We also thank Dr Roger Hunt and Dr Alistar Bonin of Western Adelaide Palliative Care for reviewing the manuscript.
None identified.