A 50-year-old woman presented to her dermatologist in 1999 with a 6-month history of recurrent pruritic scaly plaques on the abdomen, arms and hairline. The rash, which was presumed to be seborrhoeic dermatitis, improved after treatment with systemic prednisolone. No skin biopsies were taken at the time.
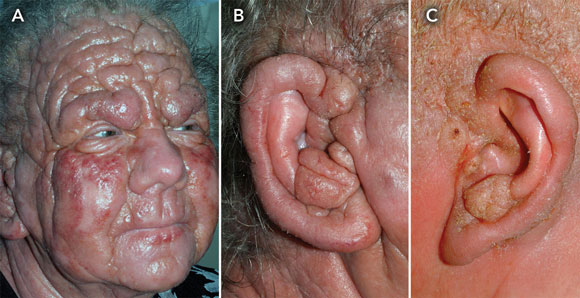
In 2004, she developed a leonine facies (Box, A), widespread erythroderma, alopecia, generalised peripheral lymphadenopathy, hyperkeratosis of the palms, and bilateral swollen pinnae with otorrhoea (Box, B).
Radical palliative radiotherapy to the head and neck improved her leonine facies and otitis externa (Box, C).
The patient died in 2006, 8 years after initial presentation.
Online responses are no longer available. Please refer to our instructions for authors page for more information.





Acknowledgements: We would like to thank Di Vickers, Medical Photographer, and Robyn Proctor, Nurse, Department of Otolaryngology, of Whangarei Hospital, New Zealand.